Arthritis is one of the most common causes of pain and disability in the UK, affecting millions of people across all age groups. Yet despite how widespread it is, many people still use the word arthritis as if it refers to a single condition. In reality, arthritis is an umbrella term covering more than 100 different joint disorders. Among them, osteoarthritis and rheumatoid arthritis are by far the most common—and the most frequently confused.
Understanding the difference between these two conditions is crucial. While both can cause joint pain, stiffness and reduced mobility, they have very different causes, progressions and treatment approaches. For people in the UK navigating GP appointments, referrals, or managing symptoms day to day, knowing what sets these conditions apart can lead to earlier diagnosis, better treatment and improved quality of life.
This article explains osteoarthritis and rheumatoid arthritis in clear, practical terms, highlighting how they differ, how they are diagnosed, and how people in the UK can manage them effectively.
What Is Arthritis? A Brief Overview
Arthritis simply means inflammation of the joints. Symptoms commonly include:
- joint pain
- stiffness
- swelling
- reduced range of movement
However, the underlying causes vary widely. Some forms of arthritis are caused by wear and tear, while others are driven by immune system dysfunction. Osteoarthritis and rheumatoid arthritis sit on opposite ends of this spectrum.
Osteoarthritis: The Wear-and-Tear Condition
What Is Osteoarthritis?
Osteoarthritis (OA) is the most common form of arthritis in the UK. It is a degenerative joint condition, meaning it develops gradually as joint tissues break down over time.
In a healthy joint, cartilage acts as a smooth cushion between bones. In osteoarthritis:
- cartilage becomes thinner and rougher
- bones may rub together
- joint shape can change
- movement becomes painful and stiff
Although often described as “wear and tear”, osteoarthritis is more complex than simple ageing and can affect younger people too.
Who Gets Osteoarthritis?
Osteoarthritis is more common in:
- people over 45
- women, particularly after menopause
- individuals with previous joint injuries
- people who are overweight
- those with physically demanding jobs
In the UK, knees, hips, hands and the spine are the most commonly affected joints.
Symptoms of Osteoarthritis
Symptoms usually develop slowly and worsen over time. Common signs include:
- pain during or after movement
- stiffness, especially after rest or in the morning
- reduced flexibility
- a grating or cracking sensation
- mild swelling
Pain often improves with rest and worsens with activity.
What Causes Osteoarthritis?
Several factors contribute to osteoarthritis:
- age-related cartilage changes
- joint injuries or surgery
- repetitive strain
- muscle weakness around joints
- genetics
Osteoarthritis is not primarily an inflammatory disease, though inflammation can occur as the condition progresses.
Rheumatoid Arthritis: An Autoimmune Condition
What Is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disease. Unlike osteoarthritis, it is not caused by joint wear and tear. Instead, the immune system mistakenly attacks the lining of the joints, causing inflammation.
Over time, this inflammation can:
- damage cartilage and bone
- deform joints
- affect other organs
Rheumatoid arthritis is a systemic condition, meaning it affects the whole body—not just the joints.
Who Gets Rheumatoid Arthritis?
Rheumatoid arthritis:
- can develop at any age
- is more common in women
- often begins between ages 30 and 50
In the UK, around 1 in 100 people live with rheumatoid arthritis.
Symptoms of Rheumatoid Arthritis
RA symptoms tend to appear more suddenly and are often symmetrical, affecting the same joints on both sides of the body. Common symptoms include:
- joint pain and swelling
- prolonged morning stiffness (often over an hour)
- fatigue
- flu-like symptoms
- warmth and redness in joints
Small joints of the hands, wrists and feet are often affected first.
What Causes Rheumatoid Arthritis?
The exact cause is unknown, but contributing factors include:
- genetic predisposition
- hormonal influences
- environmental triggers
- smoking
Unlike osteoarthritis, rheumatoid arthritis is driven by ongoing inflammation.
Key Differences Between Osteoarthritis and Rheumatoid Arthritis
Cause
- Osteoarthritis: mechanical wear and joint degeneration
- Rheumatoid arthritis: autoimmune inflammation
Onset
- Osteoarthritis: gradual, develops over years
- Rheumatoid arthritis: can be sudden or progress quickly
Age of Onset
- Osteoarthritis: usually later in life
- Rheumatoid arthritis: can start at any age
Joint Involvement
- Osteoarthritis: often affects one joint or one side
- Rheumatoid arthritis: usually symmetrical
Morning Stiffness
- Osteoarthritis: short-lived
- Rheumatoid arthritis: prolonged
Systemic Symptoms
- Osteoarthritis: limited to joints
- Rheumatoid arthritis: affects the whole body
Diagnosis in the UK Healthcare System
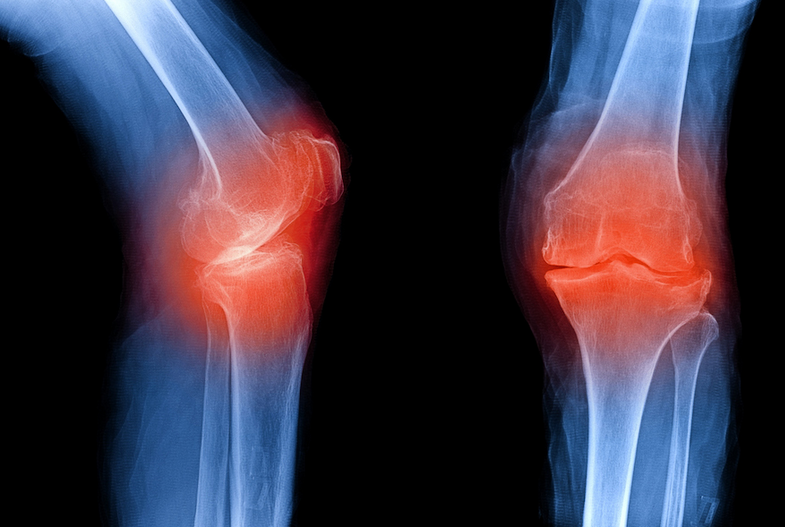
Osteoarthritis Diagnosis
Diagnosis is often based on:
- medical history
- physical examination
- symptoms
X-rays may show cartilage loss or bone changes, but imaging is not always necessary.
Rheumatoid Arthritis Diagnosis
RA diagnosis involves:
- blood tests (e.g. rheumatoid factor, anti-CCP)
- inflammation markers
- imaging scans
Early referral to a rheumatologist is critical, as early treatment can prevent long-term joint damage.
Treatment Approaches: How They Differ
Treating Osteoarthritis
There is currently no cure, but symptoms can be managed effectively.
Common approaches include:
- exercise and physiotherapy
- weight management
- pain relief medication
- joint supports
- lifestyle adjustments
In severe cases, joint replacement surgery may be considered.
Treating Rheumatoid Arthritis
RA treatment focuses on controlling inflammation and slowing disease progression.
Options include:
- disease-modifying antirheumatic drugs (DMARDs)
- biologic therapies
- anti-inflammatory medication
- physiotherapy and occupational therapy
Early treatment is key to preventing irreversible joint damage.
The Role of Exercise in Both Conditions
Exercise is essential for both forms of arthritis, though approaches differ.
For Osteoarthritis
- strengthens muscles
- reduces joint load
- improves flexibility
For Rheumatoid Arthritis
- maintains mobility
- reduces fatigue
- supports mental wellbeing
Low-impact activities such as walking, swimming and cycling are widely recommended in the UK.
Lifestyle Factors That Matter
Weight Management
Excess weight increases pressure on joints, particularly in osteoarthritis.
Smoking
Strongly linked to rheumatoid arthritis development and severity.
Diet
Anti-inflammatory eating patterns may help manage symptoms, especially in RA.
Living With Arthritis in the UK
Support is available through:
- NHS services
- physiotherapy referrals
- occupational therapy
- arthritis charities and support groups
Workplace adjustments and disability support may also be available under UK employment law.
Can You Have Both Conditions?
Yes. Some people develop both osteoarthritis and rheumatoid arthritis, particularly as they age. Each condition requires tailored management.
When to See a GP
Seek medical advice if you experience:
- persistent joint pain
- swelling or warmth
- prolonged morning stiffness
- unexplained fatigue
Early diagnosis leads to better outcomes, especially for rheumatoid arthritis.
Common Myths About Arthritis
“Arthritis only affects older people”
False. Rheumatoid arthritis can affect young adults.
“Exercise makes arthritis worse”
False. Appropriate exercise protects joints.
“Nothing can be done”
False. Effective treatments exist for both conditions.
Looking Ahead: Research and Hope
Medical research in the UK continues to improve treatment options, particularly for rheumatoid arthritis. Earlier diagnosis and personalised medicine are transforming outcomes.
Conclusion: Why Understanding the Difference Matters
Osteoarthritis and rheumatoid arthritis may share symptoms, but they are fundamentally different conditions. One is driven by joint degeneration, the other by immune system dysfunction. Understanding which type you have—or may be developing—can make a profound difference to treatment, symptom control and long-term joint health.
For people across the UK, recognising early signs, seeking timely medical advice and adopting supportive lifestyle changes can help maintain independence and quality of life. Sanoflex Forte Arthritis does not have to define your future—but understanding it is the first step towards managing it effectively.https://www.sano-flex.org.uk/

